Deep neck infections and abscess: case series and up to date commentary
Introduction
Deep neck infections are rapidly progressive, usually bacterial infections abscess of the neck, representing life threatening medical conditions. The disease course is from: (I) localization of the findings; (II) the particular spectrum of pathogens; (III) the age and comorbidities e.g., diabetes mellitus, immunosuppression the patient depends (1,2) (Figure 1).
The greatest risk is by the appearance of accompanying edema of the larynx with acute dyspnea the progression of inflammation inferiorly and favoring a mediastinitis with corresponding mortality and morbidity. Rapidly progressive course of the disease with severe general symptoms (possible risk of necrotizing fasciitis). Mortality neck abscess 2.5% mortality fasciitis 20%. Triggers are often infections of the pharynx (Figures 2-6). Odontogenic infection or abscess lymphadenitis, as well as traumatic lesions of the mucosa or upper respiratory tract of the esophagus, infections of the salivary glands, thyroid and also of the outer and middle ear (3).
Major symptoms
- Performance status temperature increase;
- Pain-related posture of the neck;
- Localized pain on pressure, possibly skin redness, warmth;
- Swallowing, partly, severe dysphagia;
- Lockjaw dyspnea, stridor, hoarseness.
Diagnosis
- History (often of failed therapeutic trial of oral antibiotics without improvement of symptoms);
- Typical symptoms;
- Clinical examination (inspection, Halspalpation, oropharyngeal inspection, laryngoscopy);
- Laboratory tests [leukocytosis, C-reactive protein (CRP) increase, procalcitonin increase];
- Imaging techniques.
- Sonography of the neck soft tissues;
- Computed tomography (CT) of the neck;
- With IV contrast administration;
- Magnetic resonance imaging.
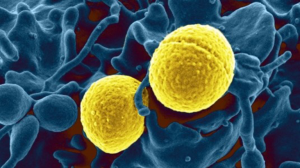
Broad spectrum of pathogens
- Bacterial infections (37% staphylococci, streptococci 29%, anaerobes, toxoplasmosis, brucellosis);
- Tuberculosis;
- Mycoses;
- Viruses (for example, CMV, HIV);
- Inflammatory diseases (sarcoidosis, Kawasaki disease);
- Parasites and other.
Therapy recommendations
Drugs
- High-dose systemic broad-spectrum antibiotics;
- Aminopenicillins + beta-lactamase inhibitor;
- Cephalosporins 2nd + 3rd generation;
- Metronidazole, clindamycin;
- In immunosuppressive underlying illness imipenem or meropenem.
Interventional therapy
- Immediate surgical reconstruction (including possibly TE) with generous opening of sternocleidomastoid (possibly combined transoral + from the outside) intraoperative swab collection;
- Insertion of drains (Redon, Penrose, rubber flap), postoperative wound daily rinses with local disinfection solutions;
- Postoperative intensive monitoring in pronounced edema hypopharyngeal or laryngeal in case of difficult extubation (4,5);
- Primary or secondary transient tracheostomy for airway.
Complications
- Edema laryngeal or hypopharyngeal;
- Mediastinitis;
- Emphysema;
- Fistula;
- Thrombophlebitis of the internal jugular vein (Lemierre’s syndrome);
- Sepsis;
- Endocarditis;
- Meningitis;
- Arthritis;
- Intracranial complications.
Case 1
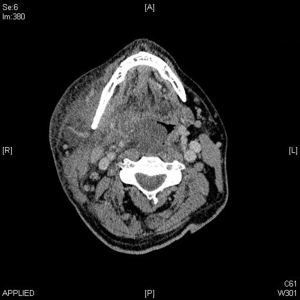
A 52-year-old patient with neck pain since 3 days with progressive swelling in the left side of the neck. Skin redness, warmth, moderate trismus, no fever. CRP elevation: 179.6 mg/L. CT-neck with KM = lymph node conglomerate below the M. scm., In the rear cervical space left (level HWK 3/4), central melting down as a sign of a possible initial inflammation (Figures 7-9).
Neck exploration left in ITN Insert a Penrose drain which was medial to the M. placed sternocleidomastoideus and was fixed by suture. Postoperative wound daily rinses with e.g., Braunol solution. Intravenous antibiotics (IV Abx) coverage with ampicillin/sulbactam + metronidazole. Smear result: streptococcus pyogenes. No complications were observed upon follow up.
Case 2
A 60-year-old patient with a 2-day acute swelling of the left sternocleidomastoid region. Inflammatory laboratory findings of CRP: 125 mg/L, no leukocytosis, afternoon recording initially no dyspnea, laryngoscopically normal. Sonographically no melting. He was hospitalized for IV Abx antiinflammatory therapy and monitoring. Overnight progressive clinical deterioration I.P. with a pronounced swelling and redness of the entire left side of the neck down to the jugular region. Moreover, hoarseness and dyspnea. Laryngoscopically: substantial edematous swelling of the left wall of the pharynx with relocation of paraglottic space and infiltration of the left vallecula (Figure 10).
Case 3
A 49-year-old patient with pre-existing MRSA colonization after paranasal sinus surgery. Since 3 days due to a right-sided neck swelling with dual antiinflammatory medical treatment oral antibiotic treatment with amoxicillin (1 g). Lockjaw, extensive swelling, redness of the right side of the neck, in partnership with Regio gland and submandibular right were observed. No fever, no dyspnoea leukocytosis: 14.9×10/µL, procalcitonin to 0.2 g/L (normal range ≤0.06 µg/L) (Figure 11).
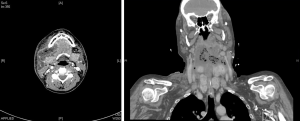
In CT-neck with KM inflammation of the entire right side of Halskompartimente the skull base to the jugular reaching with the transition to the left side and the anterior floor of the mouth to the left, starting from a tonsillogenen parapharyngeal abscess right (Figures 11-13).
Surgical exploration
Deep neck exploration right neck area, insert multiple cervical Penrose drains in extensive necrotizing area. Intravenous tazobactam was administered. Intensive care monitoring and daily wound rinses were performed. Degree of 12 days postoperatively only moderately decreased, so that a consecutive tracheotomy in dyspnea was required with renewed neck revision.
Case 4
A 56-year-old patient with acute dyspnea, fever. Endoscopic prominent swelling in the entire left rear wall of the pharynx with increased CRP, no leukocytosis no derailment of known diabetes mellitus (ketoacidotic coma), thyrotoxic crisis, hypertensive derailment, warfarin therapy in arrhythmia. Stabilization of the general condition, ICU administration. In CT pronounced left stressed phlegmonous inflammation with air pockets until after retropharyngeal (Figures 12,13).
Therapy
- Pharyngoscopy in ITN, neck exploration left, with insert several Redon drainages;
- Primary tracheotomy;
- Cover with anaerobic effective IV Abx-clindamycin + tazobac;
- In smear Streptococcus constellatus detection.
One week postoperatively occurred despite improvement of AZ and regression of infection parameters in clinically acute prominence and redness supraclavicular right (contralateral). In the CT control just yet Verhalt ipsilateral retropharyngeal or paravertebral. Renewed exploration neck bilaterally with drainage of paravertebral and retropharyngeal spaces necessary (6-9).
Conclusions
It is known that deep neck infections are considered a medical and surgical emergency. The clinical symptoms and condition severity of DCA vary according to different age groups, the location of the infection and a higher incidence of comorbidity in adults. DCA in adults usually has multi-space involvement, leads to complications and it is usually more serious than that in children. Deep neck space infection (DNSI) still remains a common and challenging disease for clinicians, and is considered an emergency. Special attention should be given to high-risk groups such as elderly, diabetics and patients with underlying systemic diseases (10). Upon admission, intravenous administration of empirical antibiotic therapy should be initiated and should be updated later according to the culture and sensitivity report (11-15). Recommendations indicate that all patients with a significant abscess on the CT scan should have surgical intervention. It has been observed that in developing countries, tobacco chewing, poor oral hygiene, lack of adequate nutrition and smoking has led to an increased prevalence of dental and periodontal diseases. Moreover, it has been observed that prevention of DNSI can be achieved by making the population aware of dental and oral hygiene.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Informed Consent: Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
References
- Kataria G, Saxena A, Bhagat S, et al. Deep Neck Space Infections: A Study of 76 Cases. Iran J Otorhinolaryngol 2015;27:293-9. [PubMed]
- Lawrence R, Bateman N. Controversies in the management of deep neck space infection (dnsi) in children: an evidence-based review. Clin Otolaryngol 2017;42:156-63. [Crossref] [PubMed]
- Brito TP, Hazboun IM, Fernandes FL, et al. Deep neck abscesses: study of 101 cases. Braz J Otorhinolaryngol 2017;83:341-8. [PubMed]
- Lakshmi Narayana M, Azeem Mohiyuddin SM, Mohammadi K, et al. Parotid abscess in children - A tertiary rural hospital experience. Int J Pediatr Otorhinolaryngol 2015;79:1988-90. [Crossref] [PubMed]
- Shah A, Ahmed I, Hassan S, et al. Evaluation of ultrasonography as a diagnostic tool in the management of head and neck facial space infections: A clinical study. Natl J Maxillofac Surg 2015;6:55-61. [Crossref] [PubMed]
- Huang CM, Huang FL, Chien YL, et al. Deep neck infections in children. J Microbiol Immunol Infect 2015. [Epub ahead of print]. [Crossref] [PubMed]
- Metin Ö, Öz FN, Tanir G, et al. Deep neck infections in children: experience in a tertiary care center in Turkey. Turk J Pediatr 2014;56:272-9. [PubMed]
- Raffaldi I, Le Serre D, Garazzino S, et al. Diagnosis and management of deep neck infections in children: the experience of an Italian paediatric centre. J Infect Chemother 2015;21:110-3. [Crossref] [PubMed]
- Cheng J, Elden L. Children with deep space neck infections: our experience with 178 children. Otolaryngol Head Neck Surg 2013;148:1037-42. [Crossref] [PubMed]
- Keppel KL, Dorrington A. Diagnostic Considerations of Ultrasound versus Computed Tomography for Pediatric Inflammatory Neck Infections. ORL Head Neck Nurs 2015;33:15-8. [PubMed]
- Fating NS, Saikrishna D, Vijay Kumar GS, et al. Detection of Bacterial Flora in Orofacial Space Infections and Their Antibiotic Sensitivity Profile. J Maxillofac Oral Surg 2014;13:525-32. [Crossref] [PubMed]
- Yusuf E, Halewyck S, Wybo I, et al. Fusobacterium necrophorum and other Fusobacterium spp. isolated from head and neck infections: A 10-year epidemiology study in an academic hospital. Anaerobe 2015;34:120-4. [Crossref] [PubMed]
- Celakovsky P, Kalfert D, Smatanova K, et al. Bacteriology of deep neck infections: analysis of 634 patients. Aust Dent J 2015;60:212-5. [Crossref] [PubMed]
- Brook I. Fusobacterial head and neck infections in children. Int J Pediatr Otorhinolaryngol 2015;79:953-8. [Crossref] [PubMed]
- Huang L, Jiang B, Cai X, et al. Multi-Space Infections in the Head and Neck: Do Underlying Systemic Diseases Have a Predictive Role in Life-Threatening Complications? J Oral Maxillofac Surg 2015;73:1320.e1-10. [Crossref] [PubMed]
Cite this article as: Karapantzos I, Karapantzou C, Zarogoulidis P, Karanikas M, Thomaidis V, Tsiouda T. Deep neck infections and abscess: case series and up to date commentary. Ann Res Hosp 2017;1:27.