The spectrum of oral and maxillofacial surgical procedures at the National Referral Hospital in Tanzania from 2013 to 2017
Introduction
There are numerous conditions that may occur in the oral and maxillofacial (OMF) region, ranging from developmental defects, injuries, and different pathologies including both benign and malignant neoplasms (1). Thus, the scope of OMF surgery includes the diagnosis and treatment of diseases affecting the mouth, jaws, face and neck (2,3).
In modern health care systems, there is a growing emphasis on monitoring the outcomes of health intervention in general and surgical procedures in particular (2). Moreover, it has been reported that the rate of postoperative complications for patients with maxillofacial conditions is directly dependent to the waiting time from day of admission to hospital until surgical intervention (4). Yet still, reports of the overall pattern of presentation and outcome of OMF surgical procedures are quite few.
As healthcare evolves and the demands on the available facilities increase, the need for evaluating existing health systems in order to improve their efficiency becomes more obvious (5). Operating theatres’ cost constitutes a huge investment of healthcare resources, approximating one third of total hospital budget (6) hence, this necessitates assessing the efficacy of surgical services in hospitals.
Surgical audit entails a systematic and critical analysis of the quality of surgical care provided, with objectives of improving quality of care, continuing education for surgeons, and guiding appropriate use of health resources (2,7). There is limited information on the audit of OMF surgical procedures in Tanzania, and to our knowledge, only one of such audits has been documented to date, and it dates back to almost a decade. This study was therefore undertaken with an aim of reporting on the indications, pattern and types of major OMF surgical procedures carried out in a tertiary referral hospital in Tanzania.
Methods
This was a retrospective review of the hospital records of all patients who had major surgery at the Oral and Maxillofacial firm (OMS) in Muhimbili National Hospital (MNH), between January 2013 and November 2017. MNH is a tertiary hospital with a 1,500-bed capacity, and it serves as a national referral centre.
The OMS provides both outpatient and inpatient services. Patients who are to undergo surgeries under general anaesthesia (GA) are usually admitted in the wards. The wards of OMS firm admit on average around 800 patients per year. The unit performs OMF surgical procedures under GA 4 days per week, and two surgeries per day. The inclusion criterion was OMF surgical procedure carried out under GA in operating room. Procedures like incisional biopsy and extractions that happened to be carried out under GA were excluded from the study. Moreover, the procedures that were carried out in the outpatient clinics under local anaesthesia (LA) were excluded as well.
Patients’ data was retrieved from the operation register. The data collected included: the age, sex, indication for surgery, histological diagnosis (in cases of tumour or tumour like lesions) and type of surgery done. The age of patients was divided into groups of age range of 10 years, thus 0–10, 11–20 and 21–30 years up to age of 71 years and above. The conditions were grouped broadly as trauma, benign neoplasms, malignant neoplasms, tumour like conditions, infection/inflammatory and others. The data were entered into a dataset by a single researcher and data analysis was done using Statistical Package for Social Sciences (SPSS) computer program version 20 (Armonk, NY: IBM Corp). The ethical clearance for this study was sought from the Institutional Review Board of the MNH (MNH/IRB/I/2018/080). The permission to conduct this study was obtained from the OMF surgery firm of MNH.
Results
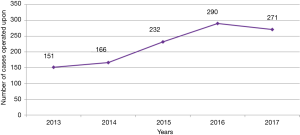
In this study, data of 1,110 patients who underwent surgical procedure under GA in the OMF region between the year 2013 and 2017 was analysed. On average, about 220 cases were operated per year, with the number of surgeries performed per year increasing from 151 cases in year 2013 to 271 cases in year 2017 (Figure 1).
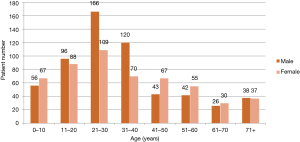
Of all the patients who underwent surgery, males were slightly more than females (52.9%, n=587). The male to female ratio was 1.1:1. The age range of the patients was from 11 days to 89 years with the mean age of 31.1±17.1 years, and the most common age groups to be managed were 21–30 years (24.8%, n=275) and 31–40 years (17.1%, n=190) (Figure 2).
Almost one third of the OMF cases managed surgically were benign neoplastic conditions (36.8%, n=409), followed by traumatic conditions (22.3%, n=248) and malignant neoplastic conditions (18.4%, n=204). The common conditions to be surgically managed in males were trauma (35.9%, n=211) followed by benign neoplasms (31.2%, n=183), while females were frequently operated for benign neoplastic conditions (43.2%, n=226) and malignant neoplastic conditions (20.8%, n=109) (Table 1).
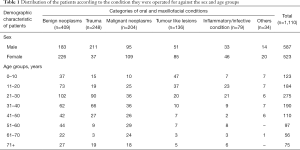
Full table
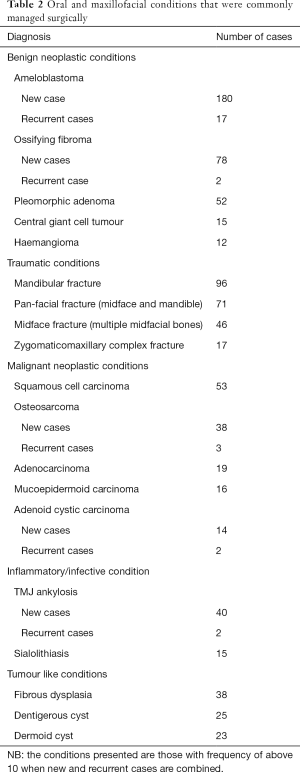
Benign neoplasms were the most common indication for majority of age groups with the exception of age group of 0–10 years, who were frequently operated for tumour like lesions, the age group 31–40 years for traumatic conditions and the age group 61–70 years for malignant neoplastic conditions (Table 1). During the study period more than 200 different types of OMF conditions were managed under GA. The most frequently operated condition was ameloblastoma (17.7%, n=197), followed by mandibular fracture (8.6%, n=96) and ossifying fibroma (7.2%, n=80) (Table 2).
Full table
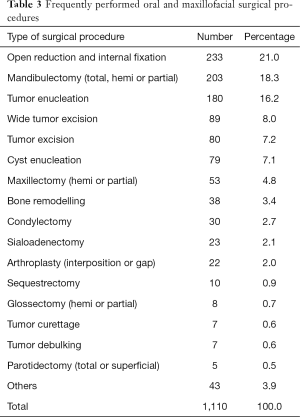
Of the primary procedures for managing the condition indicative of surgery, open reduction and internal fixation (ORIF) was the most common, followed by mandibulectomy and tumour enucleation. Of the 203 cases of mandibulectomies; partial mandibulectomy accounted for almost half of the cases (49.8%, n=101), followed by hemi-mandibulectomy (31.0%, n=63) and total mandibulectomy (19.2%, n=39). Procedures that involved maxillary bone resection (maxillectomy), were performed on 53 patients, of which hemi-maxillectomies were most common (52.8%, n=28) followed by partial maxillectomy (47.2%, n=25). Arthroplasty was performed in 22 patients and the preferred type was gap arthroplasty (77.3%, n=17) (Table 3). Secondary/additional procedures done to the patients included elective tracheostomy (n=296), mandibular reconstruction using iliac bone graft (n=40) and selective neck dissection (n=38).
Full table
Discussion
OMF region is an area that is prone to multitude of disease conditions which may be of developmental nature (e.g., vascular anomalies) or acquired nature (such as neoplasms, trauma and infections). These conditions require surgical intervention in many occasions. Thus, this retrospective study was undertaken to perform audit of OMF surgeries in our institute. Hospital based audits are said to be closest to the patients, and thus, they represent the standard of the clinical practice of a given hospital (2).
The results of current study revealed that there was almost 2-fold increase in number of cases operated per annum in the study period. A previous 6-year audit of OMF surgical procedure carried out in the same institute between 2003 and 2009 by Moshy et al. (7) reported that there were 454 cases (i.e., 75 cases per year), this indicate in general the number of OMF case operated in our institute have been steadily increasing every year. The obvious increase in number of cases operated per annum in our institute can be explained by recruitment of more trained OMF surgeons in the firm (from seven surgeons in 2009 to 14 at present). Other reasons include raised awareness about orofacial condition in general population and among clinicians, and strong efforts put by the hospital management team in ensuring accessibility to surgical armamentarium is maintained.
In this study, there were more male patients than their female counterparts. Similar results have been reported in other studies (2,5,8), however they differed from what was reported by Moshy et al. (7). The ratio of male to female differed in all the studies, and this can be attributed to difference in study design, inclusion criteria and socioeconomic status.
In general, the benign neoplastic conditions were more frequently managed surgically followed by trauma and malignant conditions. Higher prevalence of benign conditions is attributed to the fact that, benign OMF neoplasms are vast collection of different conditions; Moreover, these conditions are frequently painless and rarely interfere with function, hence patients do present much later with large lesions that cannot be managed under LA, thus requiring GA.
Ameloblastomas, ossifying fibroma and pleomorphic adenomas were the most frequently operated benign conditions. A recent study that reviewed the histological diagnosis of benign condition in our setting (9) did reveal predominance of these lesions as well. Ameloblastomas are most common benign tumours and its higher prevalence can be explained by its heterogeneous epithelial origin (9).
The management of injuries to the maxillofacial complex remains a challenge for OMF surgeons, demanding both skill and a high level of expertise (10). Similar to the findings of a study from Nigeria et al. (5), maxillofacial trauma was the second most frequent indication for surgery in this study. However, to the contrast of the current study, the maxillofacial trauma was the principle indication for surgery in other studies (2,3). Had all the traumatic conditions be managed by ORIF, trauma to orofacial region could have been leading indication for surgery in our setting. Most cases of trauma, especially mandibular fractures were managed by closed reduction under LA. Financial incapacitation among patients, limited theatre availability and limited access to required implants (metal plates and screws) were the leading reasons for opting for closed reduction.
The cases of malignant neoplasms treated surgically were just a portion of all malignant neoplastic conditions that are received in MNH. Majority of patients with malignancies do present late, thus have an advanced lesion causing severe morbidity, deformity and at times metastasis to other organs, thereby they are rendered inoperable and thus managed by palliative treatment. The common malignant condition that was managed surgically was squamous cell carcinoma. These findings are in agreement with those from other studies (2,5,11). The head and neck region is an exposed region, with many routes (i.e., ear, mouth and nose) for carcinogens to pass through frequently and in large quantities. Most of these routes are lined by epithelial cells, thus they transform to carcinomas in long term exposure to carcinogen with squamous cell carcinoma being the leading pathology.
The findings of the current study elucidate that the most frequently performed surgical procedure was ORIF of orofacial traumatic conditions. ORIF demands direct exposure of the fracture site followed by alignment of the bone segments and fixation (12). Fixation may be rigid (e.g., using plates) or semi-rigid (e.g., intra-osseous wires). When using semi-rigid method, it might be necessary to perform maxillomandibular fixation to achieve occlusion and additional support. The cases that were managed by ORIF included all those with unfavourable fracture of mandible and midfacial bone fractures. Most cases of ORIF were performed using intra-osseous wires due to limited availability of metal implants (plates and screws).
Mandibulectomy entails removal of mandible either in part or as whole. It was the second most commonly performed surgical procedure in this study, in contrast to the findings of a study from Nigeria (5) in which it was the most common procedure. Ameloblastomas being the most common indication for surgery, were managed by performing mandibulectomy since cure of ameloblastoma is undoubtedly surgical. There are various proposed treatment options for ameloblastomas ranging from conventional to radical methods of therapy. The traditional techniques involve curettage, enucleation as well as cryosurgery; while the extreme techniques are marginal, segmental as well as composite resections (13). Several studies have reported a higher recurrence rate after conservative treatment compared to radical treatment (14). Thus, in MNH, majority of ameloblastomas were treated radically (mandibulectomy). Other indications for mandibulectomy included malignant conditions such as osteosarcomas, and carcinomas that had infiltrated the mandible; hence, as part of wide tumour excision, mandibulectomy was performed.
Tumor enucleation has been defined as a surgical procedure that involves dissection of an intra-osseous cavity while preserving its integrity (14). It may also imply dissection of a well demarcated soft tissue lesion with preservation of soft tissues surrounding it. Tumor enucleation was often performed on cystic lesions (such as dentigerous cysts and dermoid cysts) and clinically well-defined tumors such as ossifying fibromas.
Management of temporomandibular joint (TMJ) ankylosis predominantly aims at providing a satisfactory mouth opening, re-establishing normal jaw function and preventing re-ossification in long term especially in children (15). A number of treatments for this condition have been described in the literature, including simple arthroplasty, interposition arthroplasty (using temporal muscle fascia, ear cartilage or alloplastic material) and reconstruction of the joint using acrylic, titanium, or autogenous material prostheses (16). Until now no single standard treatment protocol for TMJ ankylosis has been reported, as the failure rate (determined as re-ankylosis) still remains high (17). In the institute where the study was carried out, the most preferred methods includes gap arthroplasty, interpositional arthroplasty (using temporal muscle fascia) and condylectomy.
In the current study, the most frequently performed secondary procedures included elective tracheostomy, mandibular reconstruction and selective neck dissection. The main indications for elective tracheostomy included difficult intubation in conditions such as TMJ ankylosis and massive maxillofacial tumour and for maintaining airway in the postoperative period in cases of mandibulectomy and neck dissection. In developed world, advanced intubation techniques such as fibreoptic intubation or video laryngoscopy are used in cases of difficult intubation, however in low income counties such advance technique are scarce, thus tracheostomy becomes the only best option. The risk of failure of maintaining airway post operatively in upper aero digestive surgeries is high, and this can be attributed to post-operative oedema and also falling back of tongue due to loss of hard tissue support. Use of tracheostomy to secure the airway post-surgery has been documented in literature as well (18). Tracheostomy avoids the hazards of extubation and airway oedema in the immediate post-operative period (19). Due to lack of data in the literature dealing with postoperative airway management and complications after OMF surgeries, the decision regarding whether or not a tracheostomy is needed at the time of these surgeries is often dictated by the surgeon’s training and experience (20).
Reconstruction of hard tissue ablative defects was done for mandibular defects alone, however, in our setting, iliac bone grafts and reconstruction plates combination was a method of choice, unlike use of rib grafts as reported by Ibikunle et al. (5). The frequency of performing reconstructive surgeries is fairly low in our institute, whereby only about 20% of the patient who had mandibulectomy procedure had reconstruction of the mandible. The fewer cases of reconstruction can be attributed low economic empowerment of most of the patients, as majority of the patients attending MNH are usually in the lower and intermediate socio-economic group hence cannot afford the charges of surgery.
A few limitations could be acknowledged in the present study. Firstly, our study population represents a specific study group limited to only those undergoing OMF surgery procedures under GA. Secondly, there were some operation lists that had been missing.
Overall, the present study cast the light on the spectrum of OMF surgeries that are performed in our institute. Results of this study will aid the relevant authorities to make appropriate evidence-based plans and decisions during procurement of materials needed for managing patients with OMF conditions in future.
Conclusions
There has been an annual increase in number of OMF surgical procedures performed in our institute. Benign neoplastic conditions are the most common indication for OMF surgeries, with ameloblastoma being the commonest pathological condition. The frequently performed OMF procedure under GA was ORIF.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
Ethical Statement: The ethical clearance for this study was sought from the Institutional Review Board of the Muhimbili National Hospital (MNH/IRB/I/2018/080). The permission to conduct this study was obtained from the Oral and maxillofacial surgery firm of Muhimbili National Hospital.
References
- Sohal KS, Shubi F. Early Post-Operative Complications in Surgeries Pertaining Oral and Maxillofacial Region in MNH, Tanzania. Surg Sci 2015;6:470-7. [Crossref]
- Islam MA, Haider IA, Uzzaman MH, et al. One Year Audit of In Patient Department of Oral and Maxillofacial Surgery, Dhaka Dental College Hospital. J Maxillofac Oral Surg 2016;15:229-35. [Crossref] [PubMed]
- Adebayo ET, Ajike S, Abite M. Audit of oral and maxillofacial surgical conditions seen at Port Harcourt, Nigeria. Ann Afr Med 2008;7:29-34. [Crossref] [PubMed]
- Gazal G. Evaluation of the effectiveness of early or delayed treatment upon healing of mandibular fractures: A retrospective study. Eur J Dent 2015;9:87-91. [Crossref] [PubMed]
- Ibikunle AA, Taiwo AO, Braimah RO. A 5-year audit of major maxillofacial surgeries at Usmanu Danfodiyo university teaching hospital, Nigeria. BMC Health Serv Res 2018;18:416. [Crossref] [PubMed]
- Stavrou G, Panidis S, Tsouskas J, et al. An audit of operating room time utilization in a teaching hospital: is there a place for improvement? ISRN Surg 2014;2014:431740. [Crossref] [PubMed]
- Moshy J, Hamza O, Moshiro C. An Audit of 6 years of Oral and Maxillofacial Surgical Conditions admitted for Interventional Treatment at Muhimbili National Hospital, Dar es Salaam – Tanzania. East Cent Afr J Surg 2012;17:95-101.
- Rehman B, Din QU. Two years audit of maxillofacial surgery department at Khyber college of dentistry, Peshawar. Pakistan Oral Dent J 2009;29:13-8.
- Moshy JR, Sohal KS. The types, incidence and demographic distribution of benign oral and maxillofacial neoplasms among patients attending Muhimbili National Hospital in Tanzania, 2008-2013. Tanzan J Health Res 2016;18. [Crossref]
- Malik S, Singh G. Incidence of maxillofacial trauma in Sonepat (Haryana), India. Int J Med Dent 2013;3:80-9.
- Nwashindi A, Otasowie DO. A 2-year appraisal of orofacial neoplasms in a Nigerian hospital. Int J Infect Trop Dis 2014;1:42-50. [Crossref]
- Nasser M, Pandis N, Fleming PS, Fedorowicz Z, Ellis E, Ali K. Interventions for the management of mandibular fractures. Cochrane Database Syst Rev 2013.CD006087. [PubMed]
- Roy I, Louis A, Verma A, et al. Effective management of ameloblastoma : A review. Int J Contemp Dent Med Rev 2015;2014. [Crossref]
- Laborde A, Nicot R, Wojcik T, et al. Ameloblastoma of the jaws: Management and recurrence rate. Eur Ann Otorhinolaryngol Head Neck Dis 2017;134:7-11. [Crossref] [PubMed]
- Güven O. A clinical study on temporomandibular joint ankylosis in children. J Craniofac Surg 2008;19:1263-9. [Crossref] [PubMed]
- Vasconcelos BC, Porto GG, Bessa-Nogueira RV. Temporo mandibular joint ankylosis. Braz J Otorhinolaryngol 2008;74:34-8. [Crossref] [PubMed]
- Sporniak-Tutak K, Janiszewska-Olszowska J, Kowalczyk R. Management of temporomandibular ankylosis--compromise or individualization--a literature review. Med Sci Monit 2011;17:RA111-6. [Crossref] [PubMed]
- Chukwuneke FN, Ajuzieogu O, Chukwuka A, et al. Surgical challenges in the treatment of advanced cases of ameloblastoma in the developing world: The authors' experience. Int J Oral Maxillofac Surg 2010;39:150-5. [Crossref] [PubMed]
- White MC, Horner KC, Lai PS. Retrospective Review of the Anaesthetic Management of Maxillectomies and Mandibulectomies for Benign Tumours in Sub-Saharan Africa. PLoS One 2016;11:e0165090. [Crossref] [PubMed]
- Lin HS, Wang D, Fee WE, et al. Airway management after maxillectomy: routine tracheostomy is unnecessary. Laryngoscope 2003;113:929-32. [Crossref] [PubMed]
Cite this article as: Moshy JR, Sohal KS, Shaban SD, Owibingire SS, Shubi FM, Mtenga AA. The spectrum of oral and maxillofacial surgical procedures at the National Referral Hospital in Tanzania from 2013 to 2017. Ann Res Hosp 2019;3:3.